Psilocybin: Is it Really a Magical Solution?
You may have heard of psilocybin, the psychoactive compound in hallucinogenic ‘magic’ mushrooms. The therapeutic potentials of psilocybin are far reaching; could psilocybin be the magical solution for treating mood and substance use disorders (SUD)?
Psilocybin containing mushrooms can grow worldwide and appear to be ubiquitous across many cultures. The most common strain used is Psilocybe cubensis. These mushrooms have been used for recreational, spiritual, and religious purposes, which are evidenced by anecdotal reports and scientific studies. Since the use of psilocybin has largely been associated with the ‘hippie’ counterculture movement, there is still a lingering negative stigma surrounding psychedelics. In addition, psilocybin was classified as a Schedule I substance in the mid 20th century – effectively putting the research delving into the therapeutic potential psilocybin could bring to millions of people on hold.
What is Psilocybin’s Mechanism of Action?
Ingestion of psilocybin can cause euphoria, and visual and auditory hallucinations, more colloquially known as ‘trips’. A common misconception is that psilocybin has psychotomimetic effects – this is not the case. First, psilocybin must be metabolised to psilocin, the active compound responsible for its effects. Psilocin can be found 20 – 40 minutes after taking psilocybin. Psilocybin is quickly converted to its metabolite in the stomach or via first pass metabolism, has a bioavailability of around 50%, and a half life of 2.5 hours.
Psilocin acts as an agonist at the serotonin type 2A (5 HT2A) receptors, leading to hallucinogenic effects which downstream mediates an antidepressant and anti anxiety effect (Figure 1). Psilocybin and psilocin do not interact with the dopamine D2 receptors. While the exact mechanisms of psilocin’s actions are not fully understood, it is thought that psilocin could reduce the hyperactivation of the medial prefrontal cortex. Psilocin could mediate its antidepressant effects via the prefrontal and limbic brain regions, including the amygdala. Unlike mescaline and lysergic acid diethylamide (LSD), there is no evidence to suggest that psilocybin alters circulating oxytocin. Psilocin may exert analgesic effects by interacting with nociceptive and antinociceptive pathways.
Psilocin influences the brain’s dynamics and functional connectivity, particularly between the cortex and thalamus. It is thought to affect associative networks and sensory function networks by acting on the serotonergic system. Preliminary data suggest these changes in brain activity and the beneficial effects of psilocybin assisted psychotherapy in reducing symptoms of major depressive disorder (MDD) can last for up to 12 months. Similarly, in patients with life-threatening cancer (N=56), preliminary data showed that improvements in anxiety may be long-term as 80% of patients with life-threatening cancer had sustained decreases in both depressed mood and anxiety at 6 months after psilocybin consumption. Further research is required to understand the duration of these neurological changes after psilocybin consumption, which will impact dosing frequency.
Figure 1:
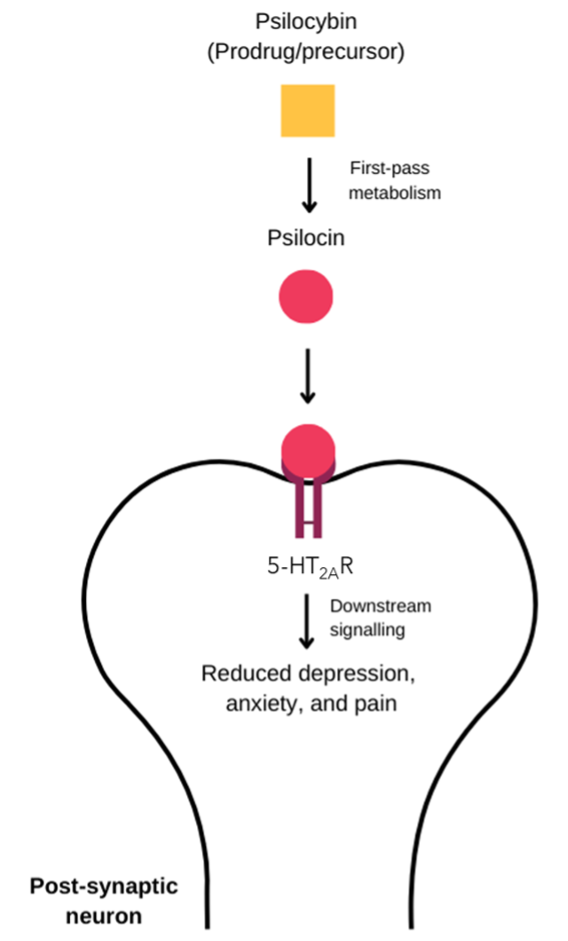
Psilocybin’s mechanism of action. When psilocybin is ingested, it is broken down by first pass metabolism into the active form, psilocin. Psilocin can then bind to the 5 HT2AR on the post synaptic neuron triggering downstream signalling leading to decreases in depression, anxiety, and pain.
5 HT2A R; Serotonin 5 HT2A receptor.
The Unmet Need in Psychiatric Conditions
Over 1 billion people worldwide have been diagnosed with psychiatric conditions. Psychiatric conditions are the leading cause of disability worldwide and increase the risk of mortality. In the United States (US), psychiatric illnesses cost the economy $1.6 trillion in 2019. It is well documented that quality of life (QoL) is lower in patients with a psychiatric condition than the general population. QoL decreases with increased symptom severity. Psychiatric conditions greatly impact all aspects of life and without adequate treatment can impair QoL. For example, patients with a diagnosis of MDD and generalised anxiety disorder (GAD) report lower QoL than those with a single diagnosis, suggesting the impact on QoL is accumulative. About 40% and 75% of individuals with a diagnosed anxiety disorder or MDD, respectively, experience sleep disturbances which subsequently impacts their QOL. Moreover in a study evaluating the effect of post traumatic stress disorder (PTSD) in 524 war veterans, 50% of male war veterans reported that their work was impacted by their diagnosis compared to just 16% of male war veterans without a diagnosis of PTSD. Additionally,17% of male war veterans diagnosed with PTSD reported that their ability to function as a parent was “often” or “always” impaired compared to just 4% of male war veterans without a diagnosis of PTSD.
A further challenge in psychiatric care is that a considerable proportion of patients do not respond to current treatments. For example, it is estimated that 50% of patients with GAD will not respond to a first line treatment, normally a selective serotonin reuptake inhibitor (SSRI). About 30% of patients with MDD receive a diagnosis of treatment resistant depression (TRD). TRD refers to a failure to respond to at least two antidepressant treatments when an adequate dose and duration of treatment was administered. There is a need for new and effective treatments for those patients who do not achieve an adequate response to current treatments. The use of ketamine assisted psychotherapy for the treatment of TRD has paved the way for the potential use of other psychedelics including psilocybin for the treatment of psychiatric conditions.
An Overview of the Landscape of Psilocybin Clinical Trials
There is preliminary evidence from clinical trials that psilocybin assisted therapy (the supervised administration of psilocybin) for treating depression and anxiety disorders, alongside early data to support its efficacy in reducing harmful drinking in patients with alcohol use disorders. Psilocybin could also alleviate pain, demonstrating analgesic effects for cluster (‘suicide’) headaches, chronic pain, and intractable phantom limb pain. In fact, Australia has approved psilocybin assisted psychotherapy and methylenedioxymethamphetamine (MDMA)-assisted psychotherapy in a clinical setting for PTSD and TRD.
At the time of writing, there have been 140 clinical trials researching how psilocybin works and whether it has therapeutic potential in disease (Figure 2a). The US is leading the way in clinical research regarding psilocybin. Of these clinical trials, 53% are active with just over half of the active clinical trials being Phase 2 studies (Figure 2b). Most ongoing clinical trials focus on mental illnesses, particularly MDD and SUD (Figure 2c). However, psilocybin is also being investigated as a potential treatment for indications outside of psychiatric conditions including chronic pain, functional neurological disorder, and migraines.
To truly understand whether psilocybin is a magical solution, large-scale head to head clinical trials against standard of care treatments are needed. Completed clinical trials of this nature for psilocybin are scarce as most clinical trials have/are comparing psilocybin to placebo. One of the few clinical trials compared psilocybin to escitalopram in MDD. Dr Robin Carhart-Harris, the leading investigator of the clinical trial, said that patients reported feeling "recalibrated, reset like they haven't for years" and "enjoying life". However, there was no notable difference in the depression score, a 16 item Quick Inventory of Depressive Symptomatology Self Report between psilocybin and escitalopram. The response rate was 70% in patients treated with psilocybin compared to 48% in the escitalopram group. Further large scale clinical trials are needed with comparisons to other common antidepressants e.g., citalopram to truly understand the therapeutic potential of psilocybin in MDD.
Figure 2:
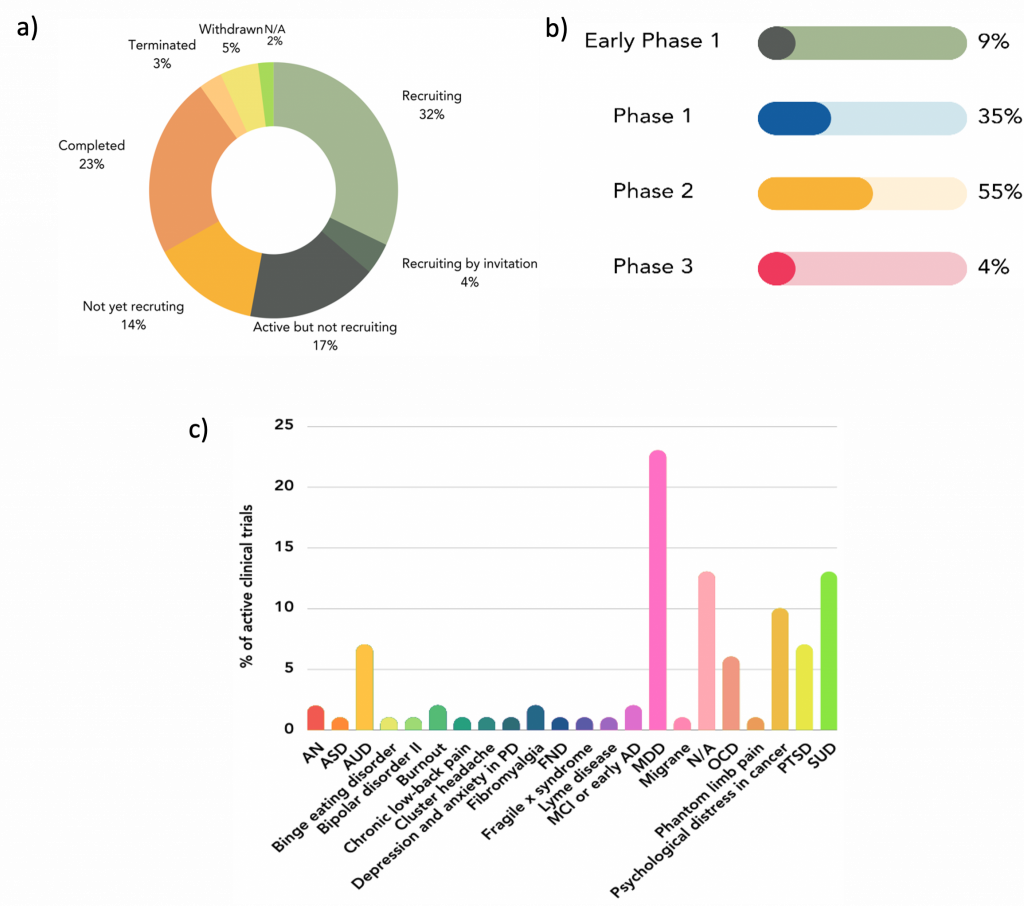
Key data regarding clinical trials for the medical use of psilocybin. *A) Status of all psilocybin clinical trials (N=140). B) Phase of all active and not yet recruiting psilocybin clinical trials (n=74).21 C) Breakdown of diseases that psilocybin is being investigated for in active and not yet recruiting clinical trials (n=74).†
*Clinical trial information is taken from ClinicalTrial.gov and was accurate as of 6th October 2023. †N/A refers to any studies that use healthy volunteers.
AD, Alzheimer’s disease; AN, anorexia nervosa; ASD, autism spectrum disorder; AUD; alcohol use disorder; FND, functional neurological disorder; MCI, mild cognitive impairment; MDD, major depressive disorder; N/A, not available; OCD, obsessive compulsive disorder; PD, Parkinson’s disease; PTSD, post-traumatic stress disorder; SUD, substance use disorder.
Psilocybin’s Safety Profile
Psilocybin is often coined the psychedelic with the most favourable safety profile as an overdose from consumption is extremely rare, has low toxicity, and has low additictiveness. The Registry of Toxic Effects of Chemical Substances (RTECS) evaluates the lowest dose known for a substance to cause a toxic effect and based on this dose assigns a therapeutic index value. The higher the therapeutic index, the safer the substance. Interestingly, RTECS assigned psilocybin a therapeutic index of 641 whereas nicotine and aspirin have lower values of 21 and 199, respectively.
Common adverse events (AEs) are summarised in Figure 3 and are exacerbated when psilocybin is consumed in conjunction with alcohol or other substances.
Figure 3:
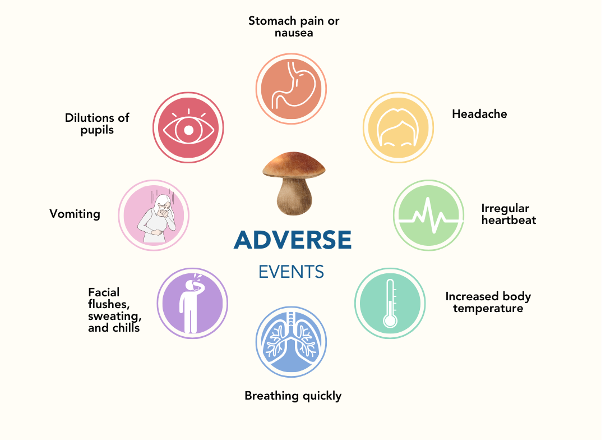
Common adverse events following consumption of psilocybin.
The Unanswered Questions in Psilocybin Research
.A question that currently remains unanswered is what, if any, drug to drug interactions does psilocybin have? As psilocybin modulates serotonin neurotransmission there is potential for drug interactions with antidepressants including SSRIs, serotonin and noradrenaline reuptake inhibitors, and tricyclic antidepressants. There is also an assumption that since LSD was found to interact with SSRIs, psilocybin will also interact with them. However, one clinical study where healthy participants (N=27) were titrated with escitalopram (20 mg) over 14 days and then administered psilocybin (25 mg) demonstrated that escitalopram did not interact with SSRIs. Pre treatment with escitalopram, had reduced bad hallucinations, anxiety, and adverse cardiovascular effects compared to those treated with psilocybin and placebo. Larger well-designed clinical trials are needed to confirm thee findings. This information would be invaluable as it would give a preliminary understanding of whether it may be possible to enhance the beneficial effects of psilocybin by combining it with conventional medications.
It is important to note that psilocybin is not the only psychedelic substance to show promise in treating psychiatric disorders. When you think of ketamine you most likely associate it with being an anaesthetic. However, ketamine also has dissociative effects and has shown promise as a treatment for MDD whilst LSD may be beneficial for treating the symptoms of PTSD. Therefore, it is important that future clinical trials evaluate psilocybin against ketamine, LSD, and other psychedelics. This information is imperative to better understand which psychedelics will be the most beneficial in certain patient populations.
Most clinical trials testing psilocybin’s efficacy have been small in size, <20 participants, and are open label. This is similar to the size of clinical trials for psychedelics in general. The strict legislation surrounding psychedelic use and the stigma of using psychedelics may account for the small clinical trial sizes. However, large scale studies are needed to provide the strong medical evidence required for policymakers to make favourable legislative changes and to help destigmatise the use of psychedelics. Such large scale clinical trials will also provide crucial and valuable insights into the optimum dose and setting for psilocybin administration. Additionally, artificial intelligence could be used alongside these trials to identify biomarkers that will predict a response to treatment with psilocybin.
The Future of Psilocybin in Medicine
Psilocybin, the mystical compound found in 'magic' mushrooms, has ignited both fascination and controversy. Historically celebrated for recreational and spiritual experiences, its classification as a Schedule I substance in the mid 20th century stifled its therapeutic potential. Psilocybin's favourable safety profile with a low overdose rate and minimal toxicity has encouraged researchers to explore its therapeutic potential. To date 140 clinical trials have been or are investigating the therapeutic potential of psilocybin. Most are focused on psychiatric conditions such as MDD. The results so far are particularly promising for MDD and offer hope to the 30% of people with MDD who have a diagnosis of TRD. However, well-designed large-scale clinical trials are needed to provide robust evidence of the medicinal benefits of psilocybin. These will help to reduce the stigma around the use of psychedelics and provide the evidence needed for policymakers to make the necessary legislative changes for psilocybin to be used therapeutically.
References
1. Sharma P, Nguyen QA, Matthews SJ, et al. Psilocybin history, action and reaction: A narrative clinical review. J Psychopharmacol. 2023;37(9):849c865.
2. Ziff S, Stern B, Lewis G, Majeed M, Gorantla VR. Analysis of Psilocybin-Assisted Therapy in Medicine: A Narrative Review. Cureus. 14(2):e21944.
3. Lowe H, Toyang N, Steele B, et al. The Therapeutic Potential of Psilocybin. Molecules. 2021;26(10):2948.
4. Nkadimeng SM, Steinmann CML, Eloff JN. Effects and safety of Psilocybe cubensis and Panaeolus cyanescens magic mushroom extracts on endothelin-1-induced hypertrophy and cell injury in cardiomyocytes. Sci Rep. 2020;10(1):22314.
5. Kraehenmann R, Preller KH, Scheidegger M, et al. Psilocybin-Induced Decrease in Amygdala Reactivity Correlates with Enhanced Positive Mood in Healthy Volunteers. Biol Psychiatry. 2015;78(8):572–581.
6. Carhart-Harris RL, Leech R, Williams TM, et al. Implications for psychedelic-assisted psychotherapy: functional magnetic resonance imaging study with psilocybin. Br J Psychiatry. 2012;200(3):238–244.
7. Ley L, Holze F, Arikci D, et al. Comparative acute effects of mescaline, lysergic acid diethylamide, and psilocybin in a randomized, double-blind, placebo-controlled cross-over study in healthy participants. Neuropsychopharmacology. 2023;48(11):1659–1667.
8. Gukasyan N, Davis AK, Barrett FS, et al. Efficacy and safety of psilocybin-assisted treatment for major depressive disorder: Prospective 12-month follow-up. J Psychopharmacol. 2022;36(2):151–158.
9. Griffiths RR, Johnson MW, Carducci MA, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double-blind trial. Journal of psychopharmacology (Oxford, England). 2016;30(12).
10. Calder AE, Hasler G. Towards an understanding of psychedelic-induced neuroplasticity. Neuropsychopharmacol. 2023;48(1):104–112.
11. Arias D, Saxena S, Verguet S. Quantifying the global burden of mental disorders and their economic value. eClinicalMedicine. 2022;54.
12. Berghöfer A, Martin L, Hense S, Weinmann S, Roll S. Quality of life in patients with severe mental illness: a cross-sectional survey in an integrated outpatient health care model. Qual Life Res. 2020;29(8):2073–2087.
13. Chellappa SL, Aeschbach D. Sleep and anxiety: From mechanisms to interventions. Sleep Med Rev. 2022;61:101583.
14. Nutt D, Wilson S, Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin Neurosci. 2008;10(3):329336.
15. Vogt D, Smith BN, Fox AB, Amoroso T, Taverna E, Schnurr PP. Consequences of PTSD for the work and family quality of life of female and male U.S. Afghanistan and Iraq War veterans. Soc Psychiatry Psychiatr Epidemiol. 2017;52(3):341352.
16. Gabriel FC, Stein AT, Melo D de O, et al. Guidelines’ recommendations for the treatment-resistant depression: A systematic review of their quality. PLOS ONE. 2023;18(2):e0281501.
17. Al-Harbi KS. Treatment-resistant depression: therapeutic trends, challenges, and future directions. Patient Prefer Adherence. 2012;6:369–388.
18. Ansara ED. Management of treatment-resistant generalized anxiety disorder. Ment Health Clin. 2020;10(6):326–334.
19. Dore J, Turnipseed B, Dwyer S, et al. Ketamine Assisted Psychotherapy (KAP): Patient Demographics, Clinical Data and Outcomes in Three Large Practices Administering Ketamine with Psychotherapy. Journal of Psychoactive Drugs. 2019;51(2):189–198.
20. Haridy R. Australia to prescribe MDMA and psilocybin for PTSD and depression in world first. Nature. 2023;619(7969):227–228.
21. ClinicalTrials.gov. Psilocybin Search Results. Available at: https://clinicaltrials.gov/search?intr=Psilocybin. Accessed: 11/10/23.
22. Carhart-Harris R, Giribaldi B, Watts R, et al. Trial of Psilocybin versus Escitalopram for Depression. N Engl J Med. 2021;384(15):1402–1411.
23. Rachel Schraer. Psilocybin: Magic mushroom compound 'promising' for depression. Available at: https://www.bbc.co.uk/news/health-56745139. Accessed:12/10/23.
24. RTECS. Registry of Toxic Effects of Chemical Substances (RTECS). Comprehensive Guide to the RTECS. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 1997.
25. Davis AK, Barrett FS, May DG, et al. Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2021;78(5):481–489.
26. Sarparast A, Thomas K, Malcolm B, Stauffer CS. Drug-drug interactions between psychiatric medications and MDMA or psilocybin: a systematic review. Psychopharmacology (Berl). 2022;239(6):1945–1976.
27. Strassman R. Human hallucinogen interactions with drugs affecting serotonergic neurotransmission.
28. Becker AM, Holze F, Grandinetti T, et al. Acute Effects of Psilocybin After Escitalopram or Placebo Pretreatment in a Randomized, Double‐Blind, Placebo‐Controlled, Crossover Study in Healthy Subjects. Clin Pharmacol Ther. 2022;111(4):886895.
29. Nutt D. Psychedelic drugs—a new era in psychiatry? Dialogues 2019;21(2):139–147.
30. Mandal S, Sinha VK, Goyal N. Efficacy of ketamine therapy in the treatment of depression. Indian J Psychiatry. 2019;61(5):480–485.
31. Shiroma PR, Thuras P, Wels J, et al. A randomized, double-blind, active placebo-controlled study of efficacy, safety, and durability of repeated vs single subanesthetic ketamine for treatment-resistant depression. Transl Psychiatry. 2020;10(1):1-9.
32. Smith-Apeldoorn SY, Veraart JK, Spijker J, Kamphuis J, Schoevers RA. Maintenance ketamine treatment for depression: a systematic review of efficacy, safety, and tolerability. Lancet Psychiatry. 2022;9(11):907–921.
33. Kargbo RB. Pioneering Changes in Psychiatry: Biomarkers, Psychedelics, and AI. ACS Med Chem Lett. 2023;14(9):1134–1137.

Author
Alice Hamilton
Project Manager and Medical Writer

